Craniopharyngioma
| Craniopharyngioma | |
|---|---|
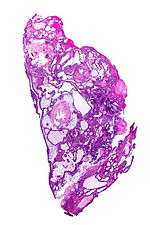 | |
| Micrograph of a craniopharyngioma (adamantinomatous). HPS stain. | |
| Classification and external resources | |
| Specialty | oncology |
| ICD-10 | D44.4 |
| ICD-9-CM | 237.0 |
| ICD-O | 9350/1 |
| DiseasesDB | 3153 |
| MedlinePlus | 000345 |
| eMedicine | radio/196 |
| Patient UK | Craniopharyngioma |
| MeSH | D003397 |
Craniopharyngioma is a type of brain tumor derived from pituitary gland embryonic tissue,[1] that occurs most commonly in children but also in men and women in their 50s and 60s.[2] People may present with bitemporal inferior quadrantanopia leading to bitemporal hemianopsia, as the tumor may compress the optic chiasm.
It has a point prevalence of approximately 2/100,000.[3]
Craniopharyngiomas are also known as Rathke pouch tumors, hypophyseal duct tumors, or adamantinomas.
Signs and symptoms
Craniopharyngioma is a rare, usually suprasellar[4] neoplasm, which may be cystic, that develops from nests of epithelium derived from Rathke's pouch.[5][6] Rathke's pouch is an embryonic precursor of the anterior pituitary.
Craniopharyngiomas are typically very slow growing tumors. They arise from the cells along the pituitary stalk, specifically from nests of odontogenic (tooth-forming) epithelium within the suprasellar/diencephalic region and, therefore, contain deposits of calcium that are evident on an x-ray. They are classified by histology as benign;[7] however, as with many brain tumors, their treatment can be difficult, and significant morbidities are associated with both the tumor and treatment.
- Balance disorder
- Dry skin
- Fatigue
- Fever
- Headache (obstructive hydrocephalus)
- Hypersomnia
- Lethargy
- Myxedema
- Nausea
- Short stature
- Polydipsia
- Polyuria (diabetes insipidus)
- Vision loss (bitemporal hemianopia)
- Vomiting
- post surgical Weight gain[8]
Diagnosis
The histologic pattern consists of nesting of squamous epithelium bordered by radially arranged cells. It is frequently accompanied by calcium deposition and may have a microscopic papillary architecture.
Two distinct types are recognized:[9][10]
- Adamantinomatous craniopharyngiomas, which resemble ameloblastomas (the most common type of odontogenic tumor), are characterized by activating CTNNB1 mutations; and,
- Papillary craniopharyngiomas are characterized by BRAFv600E mutations.[11]
In the adamantinomatous type, calcifications are visible on neuroimaging and are helpful in diagnosis. The papillary type rarely calcifies.
On macroscopic examination, craniopharyngiomas are cystic or partially cystic with solid areas. On light microscopy, the cysts are seen to be lined by stratified squamous epithelium. Keratin pearls may also be seen. The cysts are usually filled with a yellow, viscous fluid which is rich in cholesterol crystals. Of a long list of possible symptoms, the most common presentations include: headaches, growth failure, and bitemporal hemianopsia.
 CT scan showing a craniopharyngioma.
CT scan showing a craniopharyngioma. Enhanced T1 weighted MRI's of craniopharyngiomas.
Enhanced T1 weighted MRI's of craniopharyngiomas.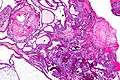 Micrograph showing the characteristic features of an adamantinomatous craniopharyngioma - cystic spaces, calcifications, and "wet" keratin. HPS stain.
Micrograph showing the characteristic features of an adamantinomatous craniopharyngioma - cystic spaces, calcifications, and "wet" keratin. HPS stain. Micrograph showing a papillary craniopharyngioma. HPS stain.
Micrograph showing a papillary craniopharyngioma. HPS stain.
Prognosis
Craniopharyngiomas are generally benign but are known to recur after resection. Recent research[12] has demonstrated a malignant (but rare) tendency of craniopharyngiomas. These malignant craniopharyngiomas are very rare, but are associated with poor prognosis.
Malignant craniopharyngioma
Craniopharyngiomas are usually successfully managed with a combination of adjuvant chemotherapy and neurosurgery. Recent research describes the rare occurrence of malignant transformations of these normally benign tumors. Malignant craniopharyngiomas can occur at any age, are slightly more common in females, and are usually of the adamantinomatous type.[12]
The malignant transformations can take years to occur (although 1 in 5 of the diagnosed cases were de novo transformations), hence the need for lengthier follow up in patients diagnosed with the more common benign forms.[12]
There was no link found between malignancy and initial chemo-radiotherapy treatment,[12] and the overall survival rate was very poor with median survival being 6 months post diagnosis of malignancy.
Treatment
Treatment generally consists of subfrontal or transsphenoidal excision. Surgery using the transsphenoidal route is often performed by a joint team of ENT and neurosurgeons. Because of the location of the craniopharyngioma near the brain and skullbase, a surgical navigation system might be used to verify the position of surgical tools during the operation.[13]
Additional radiotherapy is also used if total removal is not possible. Due to the poor outcomes associated with damage to the pituitary and hypothalamus from surgical removal and radiation, experimental therapies using intracavitary phosphorus-32, yttrium, or bleomycin delivered via an external reservoir are sometimes employed, especially in young patients. The tumor, being in the pituitary gland, can cause secondary health problems. The immune system, thyroid levels, growth hormone levels and testosterone levels can be compromised from craniopharygioma. All of the before mentioned health problems can be treated with modern medicine.[14] There is no high quality evidence looking at the use of bleomycin in this condition.[15]
The most effective treatment 'package' for the malignant craniopharyngiomas described in literature is a combination 'gross total resective' surgery with adjuvant chemo radiotherapy. The chemotherapy drugs Paclitaxel and Carboplatin have shown a clinical (but not statistical) significance in increasing the survival rate in patients who've had gross total resections of their malignant tumours.[12]
Etymology and pronunciation
The term craniopharyngioma (/ˌkreɪnioʊfəˌrɪndʒiˈoʊmə/) uses combining forms of cranio- + pharyng(i) + -oma. The connection between the cranium and the pharynx that the name implies is via the craniopharyngeal canal; during embryonic development cranial and pharyngeal structures arise from the area.
See also
References
- ↑ "craniopharyngioma" at Dorland's Medical Dictionary
- ↑ Hamid R, Sarkar S, Hossain MA, Mazumder U, Akanda NI, Parvin R (2007). "Clinical picture of craniopharyngioma in childhood". Mymensingh medical journal : MMJ. 16 (2): 123–6. PMID 17703145.
- ↑ Garnett MR, Puget S, Grill J, Sainte-Rose C (2007). "Craniopharyngioma". Orphanet journal of rare diseases. 2: 18. doi:10.1186/1750-1172-2-18. PMC 1855047
 . PMID 17425791.
. PMID 17425791. - ↑ Rodriguez FJ, Scheithauer BW, Tsunoda S, Kovacs K, Vidal S, Piepgras DG (2007). "The spectrum of malignancy in craniopharyngioma". Am. J. Surg. Pathol. 31 (7): 1020–8. doi:10.1097/PAS.0b013e31802d8a96. PMID 17592268.
- ↑ Moore, Kraig D.; Couldwell, William T. (January 15, 2000). "41. Craniopharyngioma". In Bernstein, Mark; Berger, Mitchel S. Neuro-oncology: the essentials. Endorsed by the Joint Tumor Section of the American Association of Neurological Surgeons & the Congress of Neurological Surgeons. Thieme. pp. 409–418. ISBN 978-0-86577-880-1. Retrieved August 8, 2011.
- ↑ "Endocrine Pathology". Retrieved 2009-05-08.
- ↑ Garrè ML, Cama A (2007). "Craniopharyngioma: modern concepts in pathogenesis and treatment". Curr. Opin. Pediatr. 19 (4): 471–9. doi:10.1097/MOP.0b013e3282495a22. PMID 17630614.
- ↑ Ahmet A, Blaser S, Stephens D, Guger S, Rutkas JT, Hamilton J (2006). "Weight gain in craniopharyngioma--a model for hypothalamic obesity". Journal of Pediatric Endocrinology & Metabolism : JPEM. 19 (2): 121–7. doi:10.1515/jpem.2006.19.2.121. PMID 16562584.
- ↑ Sekine S, Shibata T, Kokubu A, et al. (December 2002). "Craniopharyngiomas of adamantinomatous type harbor beta-catenin gene mutations". Am. J. Pathol. 161 (6): 1997–2001. doi:10.1016/s0002-9440(10)64477-x. PMC 1850925
 . PMID 12466115.
. PMID 12466115. - ↑ Sekine S, Takata T, Shibata T, et al. (December 2004). "Expression of enamel proteins and LEF1 in adamantinomatous craniopharyngioma: evidence for its odontogenic epithelial differentiation". Histopathology. 45 (6): 573–9. doi:10.1111/j.1365-2559.2004.02029.x. PMID 15569047.
- ↑ . 46 (2) http://www.nature.com/ng/journal/v46/n2/full/ng.2868.html. Missing or empty
|title=(help) - 1 2 3 4 5 Sofela, AA; Hettige, S; Curran, O; Bassi, S (Sep 2014). "Malignant transformation in craniopharyngiomas.". Neurosurgery. 75 (3): 306–14; discussion 314. doi:10.1227/NEU.0000000000000380. PMID 24978859.
- ↑ Use of surgical navigation for craniopharyngioma removal
- ↑ Wisoff, JH (Feb 2008). "Craniopharyngioma.". Journal of Neurosurgery. Pediatrics. 1 (2): 124–5; discussion 125. doi:10.3171/PED/2008/1/2/124. PMID 18352780.
- ↑ Zheng, J; Fang, Y; Cai, BW; Zhang, H; Liu, W; Wu, B; Xu, JG; You, C (Sep 19, 2014). "Intracystic bleomycin for cystic craniopharyngiomas in children.". The Cochrane database of systematic reviews. 9: CD008890. doi:10.1002/14651858.CD008890.pub3. PMID 25233847.
External links
- Cancer.Net: Craniopharyngioma - Childhood
- Boston Neurosurgical Foundation
- Adamantinomatous Craniopharyngioma
- Malignant transformation in craniopharyngiomas
- 194641925 at GPnotebook