Ductal carcinoma in situ
| Ductal carcinoma in situ | |
|---|---|
.jpg) | |
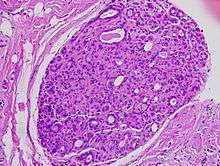
| Histopathologic image from ductal cell carcinoma in situ (DCIS) of breast. Hematoxylin and eosin stain. | |
| Classification and external resources | |
| Specialty | oncology |
| ICD-10 | D05.1 |
| MeSH | D002285 |
Ductal carcinoma in situ (DCIS), also known as intraductal carcinoma, is a pre-cancerous or non-invasive cancerous lesion of the breast.[1][2] DCIS is classified as Stage 0.[3] It rarely produces symptoms or a breast lump one can feel, and is usually detected through screening mammography.[4][5]
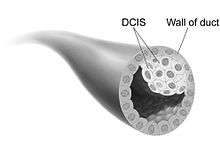
In DCIS, abnormal cells are found in the lining of one or more milk ducts in the breast. In situ means "in place" and refers to the fact that the abnormal cells have not moved out of the mammary duct and into any of the surrounding tissues in the breast ("pre-cancerous" refers to the fact that it has not yet become an invasive cancer). In some cases, DCIS may become invasive and spread to other tissues, but there is no way of determining which lesions will remain stable without treatment, and which will go on to become invasive. DCIS encompasses a wide spectrum of diseases ranging from low-grade lesions that are not life-threatening to high-grade (i.e. potentially highly aggressive) lesions.
DCIS has been classified according to the architectural pattern of the cells (solid, cribriform, papillary, and micropapillary), tumor grade (high, intermediate, and low grade), and the presence or absence of comedo histology.[6] DCIS can be detected on mammograms by examining tiny specks of calcium known as microcalcifications. Since suspicious groups of microcalcifications can appear even in the absence of DCIS, a biopsy may be necessary for diagnosis.
About 20–30% of those who do not receive treatment develop breast cancer.[7] It is the most common type of pre-cancer in women. There is some disagreement as to whether, for statistical purposes, it should be counted as a cancer: some include DCIS when calculating breast cancer statistics while others do not.[8][9]
Terminology
Ductal carcinoma in situ (DCIS) is the name given to groups of "cancerous" epithelial cells that have remained in their normal place (in situ in Latin) within the ducts and lobules of the mammary gland.[10] Clinically, it is considered a premalignant (i.e. potentially malignant) condition.[11] Each lesion contains cells that have already become biologically malignant ("cancerous") but have not yet crossed the basement membrane to invade the surrounding tissue.[10][12] When multiple lesions (known as "foci" of DCIS) are present in different quadrants of the breast, this is referred to as "multicentric" disease.[6]
For statistical purposes, some count DCIS as a "cancer", whereas others do not.[9][13] When classified as a cancer, it is referred to as a non-invasive or pre-invasive form.[10][14] The National Cancer Institute describes it as a "noninvasive condition".[9]
Signs and symptoms
_CRUK_115.svg.png)
Most of the women who develop DCIS do not experience any symptoms. The first signs and symptoms may appear if the cancer advances. Because of the lack of early symptoms, DCIS is most often detected at screening mammography.
In a few cases, DCIS may cause:
- A lump or thickening in or near the breast or under the arm
- A change in the size or shape of the breast
- Nipple discharge or nipple tenderness; the nipple may also be inverted, or pulled back into the breast
- Ridges or pitting of the breast; the skin may look like the skin of an orange
- A change in the way the skin of the breast, areola, or nipple looks or feels[15] such as warmth, swelling, redness or scaliness.[16]
Causes
The specific causes of DCIS are still unknown. The risk factors for developing this condition are similar to those for invasive breast cancer.[17]
Some women are however more prone than others to developing DCIS. Women considered at higher risks are those who have a family history of breast cancer, those who have had their periods at an early age or who have had a late menopause. Also, women who have never had children or had them late in life are also more likely to get this condition.
Long-term use of estrogen-progestin hormone replacement therapy (HRT) for more than five years after menopause, genetic mutations (BRCA1 or BRCA2 genes), atypical hyperplasia, as well as radiation exposure or exposure to certain chemicals may also contribute in the development of the condition.[18] Nonetheless, the risk of developing noninvasive cancer increases with age and it is higher in women older than 45 years.
Diagnosis
80% of cases in the United States are diagnosed by mammography screening.[19]
Treatment
There different opinions on the best treatment of DCIS.[20] Surgical removal, with or without additional radiation therapy or tamoxifen, is the recommended treatment for DCIS by the National Cancer Institute.[21] Surgery may be either a breast-conserving lumpectomy or a mastectomy (complete or partial removal of the affected breast).[22] If a lumpectomy is used it is often combined with radiation therapy.[9] Tamoxifen may be used as hormonal therapy if the cells show estrogen receptor positivity.[9] Chemotherapy is not needed for DCIS since the disease is noninvasive.[23]
While surgery reduces the risk of subsequent cancer, many people never develop cancer even without treatment and there are associated side effects.[22] There is no evidence comparing surgery with watchful waiting and some feel watchful waiting may be a reasonable option in certain cases.[22]
Radiation therapy
Use of radiation therapy after lumpectomy provides equivalent survival rates to mastectomy, although there is a slightly higher risk of recurrent disease in the same breast in the form of further DCIS or invasive breast cancer. Systematic reviews (including a Cochrane review) indicate that the addition of radiation therapy to lumpectomy reduces recurrence of DCIS or later onset of invasive breast cancer in comparison with breast-conserving surgery alone, without affecting mortality.[24][25] The Cochrane review did not find any evidence that the radiation therapy had any long-term toxic effects.[24] While the authors caution that longer follow-up will be required before a definitive conclusion can be reached regarding long-term toxicity, they point out that ongoing technical improvements should further restrict radiation exposure in healthy tissues.[24] They do recommend that comprehensive information on potential side effects is given to women who receive this treatment.[24] The addition of radiation therapy to lumpectomy appears to reduce the risk of local recurrence to approximately 12%, of which approximately half will be DCIS and half will be invasive breast cancer; the risk of recurrence is 1% for women undergoing mastectomy.[26]
Mastectomy
There is no evidence that mastectomy decreases the risk of death over a lumpectomy.[27] Mastectomy; however, may decrease the rate of the DCIS or invasive cancer occurring in the same location.[27]
Mastectomies remain a common recommendation in those with persistent microscopic involvement of margins after local excision or with a diagnosis of DCIS and evidence of suspicious, diffuse microcalcifications.[28] Some institutions that have encountered high rates of recurrent invasive cancers after mastectomy for DCIS have endorsed routine sentinel node biopsy (SNB).[29] Others reserve SNB for only certain people. Most agree that SNB should be considered with tissue diagnosis of high risk DCIS (grade III with palpable mass or larger size on imaging) as well as in people undergoing mastectomy after a core or excisional biopsy diagnosis of DCIS.[30]
Prognosis
Because DCIS is normally found early and it is treated or managed, it is difficult to say what occurs if left untreated. About 2% of women who are diagnosed with this condition and treated died within 10 years.[31] Biomarkers can identify which women who were initially diagnosed with DCIS are at high or low risk of subsequent invasive cancer.[32][33]
Epidemiology
DCIS is often detected with mammographies but can rarely be felt. With the increasing use of screening mammography, noninvasive cancers are more frequently diagnosed and now constitute 15% to 20% of all breast cancers.[34]
Cases of DCIS have increased 5 fold between 1983 and 2003 in the United States due to the introduction of screening mammography.[31] In 2009 about 62,000 cases were diagnosed.[31]
References
- ↑ Sinn, HP; Kreipe, H (May 2013). "A Brief Overview of the WHO Classification of Breast Tumors, 4th Edition, Focusing on Issues and Updates from the 3rd Edition.". Breast care (Basel, Switzerland). 8 (2): 149–154. doi:10.1159/000350774. PMID 24415964.
- ↑ Seltzer, William H. Hindle, editor ; with a foreword by Vicki (1999). Breast care: a clinical guidebook for women's primary health care providers. New York: Springer. p. 129. ISBN 9780387983486.
- ↑ Staging, Breastcancer.org
- ↑ Welch HG, Woloshin S, Schwartz LM (February 2008). "The sea of uncertainty surrounding ductal carcinoma in situ--the price of screening mammography". J. Natl. Cancer Inst. 100 (4): 228–9. doi:10.1093/jnci/djn013. PMID 18270336.
- ↑ Liberman, Laura (2005). Breast MRI. [New York]: Springer Science+Business Media, Inc. p. 164. ISBN 9780387219974.
- 1 2 Virnig BA, Shamliyan T, Tuttle TM, Kane RL, Wilt TJ (September 2009). "Diagnosis and management of ductal carcinoma in situ (DCIS)". Evidence Report/Technology Assessment. AHRQ Publication No.09-E018. (185): 1–549. PMID 20629475.
- ↑ Raphael Rubin; David S. Strayer, eds. (2008). Rubin's Pathology: clinicopathologic foundations of medicine (5. ed.). Philadelphia [u.a.]: Wolters Kluwer/Lippincott Williams & Wilkins. p. 848. ISBN 9780781795166.
- ↑ "Breast Cancer Treatment (PDQ®)". NCI. 2014-04-11. Retrieved 19 June 2014.
- 1 2 3 4 5 "Breast Cancer Treatment (PDQ®)". NCI. Retrieved 19 June 2014.
- 1 2 3 Allred DC (2010). "Ductal carcinoma in situ: terminology, classification, and natural history". Journal of the National Cancer Institute. Monographs. 2010 (41): 134–8. doi:10.1093/jncimonographs/lgq035. PMID 20956817.
- ↑ Padwal, David Hui (2011). Alexander Leung and Raj Padwal, ed. Approach to internal medicine a resource book for clinical practice (3rd ed.). New York: Springer. p. 198. ISBN 9781441965059.
- ↑ Tjandra, Joe J.; Collins, John P. (2006). "Breast surgery". In Tjandra; et al. Textbook of surgery (3rd ed.). Malden, Mass.: Blackwell Pub. p. 282. ISBN 9780470757796.
- ↑ Chang, Alfred (2007). Oncology: An Evidence-Based Approach. Springer. p. 162. ISBN 9780387310565.
- ↑ J. Saclarides (2008). Jonathan A. Myers, Keith W. Millikan, Theodore, eds. Common surgical diseases an algorithmic approach to problem solving. (2nd rev. ed.). New York: Springer. ISBN 9780387752464.
- ↑ "Breast Cancer". Retrieved 2010-06-28.
- ↑ "Signs and Symptoms". Retrieved 2010-06-28.
- ↑ "After the mammogram". Retrieved 2010-06-28.
- ↑ "Intraductal Carcinoma of the Breast". Retrieved 2010-06-28.
- ↑ "Ductal Carcinoma In Situ". cancer.gov. January 9, 2015. Retrieved 5 March 2015.
- ↑ Mannu, Gurdeep S.; Bettencourt-Silva, Joao H.; Ahmed, Farid; Cunnick, Giles (2015). "A Nationwide Cross-Sectional Survey of UK Breast Surgeons' Views on the Management of Ductal Carcinoma In Situ". International Journal of Breast Cancer. 2015: 1–7. doi:10.1155/2015/104231.
- ↑ "Ductal Carcinoma In Situ: Treatment Options for Patients With DCIS". National Cancer Institute at NIH. National Institutes of Health. 2014-07-11.
- 1 2 3 "Treatment of ductal carcinoma in situ: an uncertain harm-benefit balance.". Prescrire Int. 144 (22): 298–303. Dec 2013. PMID 24600734.
- ↑ Ductal Carcinoma in Situ (DCIS), Johns Hopkins Medicine
- 1 2 3 4 Goodwin A, Parker S, Ghersi D, Wilcken N (2013). "Post-operative radiotherapy for ductal carcinoma in situ of the breast". The Cochrane Database of Systematic Reviews. 11: CD000563. doi:10.1002/14651858.CD000563.pub7. PMID 24259251.
- ↑ Virnig, BA; Tuttle, TM; Shamliyan, T; Kane, RL (2010). "Ductal carcinoma in situ of the breast: a systematic review of incidence, treatment, and outcomes". Journal of the National Cancer Institute. 102 (3): 170–8. doi:10.1093/jnci/djp482. PMID 20071685.
- ↑ "NIH DCIS Consensus Conference Statement". National Institutes of Health. September 2009.
- 1 2 Virnig, BA; Shamliyan, T; Tuttle, TM; Kane, RL; Wilt, TJ (September 2009). "Diagnosis and management of ductal carcinoma in situ (DCIS).". Evidence report/technology assessment (185): 4. PMID 20629475.
They found women undergoing mastectomy were less likely than women undergoing lumpectomy plus radiation to experience local DCIS or invasive recurrence. Women undergoing BCS alone were also more likely to experience a local recurrence than women treated with mastectomy. We found no study showing a mortality reduction associated with mastectomy over breast conserving surgery with or without radiation.
- ↑ "Intraductal carcinoma". Retrieved 2010-06-28.
- ↑ Tan JC, McCready DR, Easson AM, Leong WL (February 2007). "Role of sentinel lymph node biopsy in ductal carcinoma-in-situ treated by mastectomy". Annals of Surgical Oncology. 14 (2): 638–45. doi:10.1245/s10434-006-9211-9. PMID 17103256.
- ↑ van Deurzen CH, Hobbelink MG, van Hillegersberg R, van Diest PJ (April 2007). "Is there an indication for sentinel node biopsy in patients with ductal carcinoma in situ of the breast? A review". European Journal of Cancer. 43 (6): 993–1001. doi:10.1016/j.ejca.2007.01.010. PMID 17300928.
- 1 2 3 Kerlikowske, K (2010). "Epidemiology of ductal carcinoma in situ.". Journal of the National Cancer Institute. Monographs. 2010 (41): 139–41. doi:10.1093/jncimonographs/lgq027. PMID 20956818.
- ↑ Kerlikowske, K.; Molinaro, A. M.; Gauthier, M. L.; Berman, H. K.; Waldman, F.; Bennington, J.; Sanchez, H.; Jimenez, C.; Stewart, K.; et al. (2010). "Biomarker Expression and Risk of Subsequent Tumors After Initial Ductal Carcinoma in Situ Diagnosis". JNCI Journal of the National Cancer Institute. 102 (9): 627–637. doi:10.1093/jnci/djq101. PMC 2864293
 . PMID 20427430.
. PMID 20427430. - ↑ Witkiewicz AK, Dasgupta A, Nguyen KH, et al. (June 2009). "Stromal caveolin-1 levels predict early DCIS progression to invasive breast cancer". Cancer Biology & Therapy. 8 (11): 1071–1079. doi:10.4161/cbt.8.11.8874. PMID 19502809.
- ↑ "Intraductal carcinoma". Retrieved 2010-06-28.