Caroli disease
| Caroli disease | |
|---|---|
|
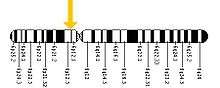
Figure 1 Biliary tract, system, or tree includes the gallbladder and the bile ducts. | |
| Classification and external resources | |
| OMIM | 263200 |
| DiseasesDB | 29874 |
| eMedicine | radio/131 ped/325 |
| MeSH | D016767 |
Caroli disease is a rare inherited disorder characterized by dilation of the intrahepatic bile ducts. There are two types of Caroli disease, the most common being the simple, or isolated case where the bile ducts are widened by ectasia. The second, more complex, cause is commonly known as Caroli Syndrome. This complex form is also linked with portal hypertension and congenital hepatic fibrosis.[1] The differences between the causes of the two cases have not yet been discovered. Caroli disease is also associated with liver failure and polycystic kidney disease. The disease affects about 1 in 1,000,000 people, with more reported cases of Caroli syndrome than of Caroli disease. [2]
Caroli disease also is known as communicating cavernous ectasia, or congenital cystic dilatation of the intrahepatic biliary tree. Caroli disease is distinct from other diseases that cause ductal dilatation caused by obstruction, in that it is not one of the many choledochal cyst derivatives. [1]
Causes
The cause appears to be genetic; the simple form is an autosomal dominant trait while the complex form is an autosomal recessive trait.[1] Females are more prone to Caroli disease than males.[3] Family history may include kidney and liver disease due to the link between Caroli Disease and ARPKD.[4] PKHD1, the gene linked to ARPKD, has been found mutated in patients with Caroli syndrome. PKHD1 is expressed primarily in the kidneys with lower levels in the liver, pancreas, and lungs, a pattern consistent with phenotype of the disease, which primarily affects the liver and kidneys.[1][4] The genetic basis for the difference between Caroli disease and Caroli syndrome has not been defined.
Signs and symptoms
The first symptoms typically include fever, intermittent abdominal pain, and hepatomegaly. Occasionally jaundice occurs. [5] Caroli disease usually occurs in the presence of other diseases, such as autosomal recessive polycystic kidney disease, cholangitis, gallstones, biliary abscess, septicemia, liver cirrhosis, renal failure, and cholangiocarcinoma (7% affected).[1] People with Caroli disease are 100 times more at risk for cholangiocarcinoma than the general population.[5] After recognizing symptoms of related diseases, Caroli disease can be diagnosed.
Morbidity is common and is caused by complications of cholangitis, sepsis, choledocholithiasis, and cholangiocarcinoma.[6] These morbid conditions often prompt the diagnosis. Portal hypertension may be present, resulting in other conditions including splenomegaly, hematemesis and melena.[4] These problems can severely affect the patient's quality of life. In a ten-year period between 1995 and 2005, only ten patients were surgically treated for Caroli disease, with an average patient age of 45.8 years.[6]
After reviewing 46 cases of Caroli disease before 1990, it was found that 21.7% of the cases were the result of an intraheptic cyst or non-obstructive biliary tree dilation, 34.7% were linked with congenital hepatic fibrosis, 13% were isolated choledochal cystic dilation, and the remaining 24.6% had a combination of all three.[7]
Diagnosis
Modern imaging techniques allow the diagnosis to be made more easily and without invasive imaging of the biliary tree.[8] Commonly the disease is limited to the left lobe of the liver. Images taken by CT-scan, X-ray, or MRI will show enlarged intrahepatic (in the liver) bile ducts due to ectasia. Using an ultrasound, tubular dilation of the bile ducts can be seen. On a CT-Scan, Caroli disease can be observed by noting the many fluid-filled, tubular structures extending to the liver.[5] A high contrast CT must be used to distinguish the difference between stones and widened ducts. Bowel gas and digestive habits make it difficult to obtain a clear sonogram, therefore, a CT scan is a good substitution. When the intrahepatic bile duct wall has protrusions, it is clearly seen as central dots or a linear streak.[9] Caroli disease is commonly diagnosed after this “central dot sign” is detected on a CT scan or ultrasound.[9] However, cholangiography is the best, and final, approach to show the enlarged bile ducts as a result of Caroli disease.
Treatment
The treatment depends on clinical features and the location of the biliary abnormality. When the disease is localized to one hepatic lobe, hepatectomy relieves symptoms and appears to remove the risk of malignancy.[10] There is good evidence that malignancy complicates Caroli disease in approximately 7% of cases.[10]
Antibiotics are used to treat the inflammation of the bile duct, and ursodeoxycholic acid for hepatolithiasis.[8] Ursodiol is given to treat cholelithiasis. In diffuse cases of Caroli disease, treatment options include conservative or endoscopic therapy, internal biliary bypass procedures and liver transplantation in carefully selected cases.[10] Surgical resection has been used successfully in patients with monolobar disease.[8] An orthotopic liver transplant is another option, used only when antibiotics have no effect, in combination with recurring cholangitis. With a liver transplant, cholangiocarcinoma is usually avoided in the long run.[11]
Family studies are necessary to determine if Caroli disease is due to inheritable causes. Regular follow-ups, including ultrasounds and liver biopsies, are performed.
Prognosis
Mortality is indirect and caused by complications. After cholangitis occurs, patients typically die within approximately 5–10 years.[2]
Epidemiology
Caroli disease is typically found in Asia and diagnosed in persons under the age of 22. Cases have also been found in both infants and adults. As medical imaging technology improves, diagnostic age decreases.
History
Jacques Caroli, a gastroenterologist, first described a rare congenital condition in 1958 in Paris, France. [3][12] He described it as "nonobstructive saccular or fusiform multi-focal segmental dilatation of the intra-hepatic bile ducts"; basically, he observed cavernous ectasia in the biliary tree causing a chronic, often life-threatening hepatobiliary disease. [13] Caroli, born in France in 1902, learned and practiced medicine in Angers. After World War II he was chief of service for 30 years at Saint-Antoine in Paris. Before dying in 1979, he was honored with the rank of commander in the Legion of Honour in 1976.[12]
References
- 1 2 3 4 5 Karim B (August 2007). "Caroli's Disease Case Reports" (PDF). Indian Pediatrics. 41 (8): 848–50. PMID 15347876.
- 1 2 Romano WJ: Caroli Disease at eMedicine
- 1 2 Kahn, Charles E, Jr. January 2003. Collaborative Hypertext of Radiology. Medical College of Wisconsin. Archived September 29, 2008, at the Wayback Machine.
- 1 2 3 Friedman JR: Caroli Disease at eMedicine
- 1 2 3 "Carolis disease". Medcyclopaedia. GE.
- 1 2 Lendoire J, Schelotto PB, Rodríguez JA, et al. (2007). "Bile duct cyst type V (Caroli's disease): surgical strategy and results". HPB (Oxford). 9 (4): 281–4. doi:10.1080/13651820701329258. PMC 2215397
 . PMID 18345305.
. PMID 18345305. - ↑ Choi BI, Yeon KM, Kim SH, Han MC (1 January 1990). "Caroli disease: central dot sign in CT". Radiology. 174 (1): 161–3. doi:10.1148/radiology.174.1.2294544. PMID 2294544.
- 1 2 3 Ananthakrishnan AN, Saeian K (April 2007). "Caroli's disease: identification and treatment strategy". Curr Gastroenterol Rep. 9 (2): 151–5. doi:10.1007/s11894-007-0010-7. PMID 17418061.
- 1 2 Chiba T, Shinozaki M, Kato S, Goto N, Fujimoto H, Kondo F (March 2002). "Caroli's disease: central dot sign re-examined by CT arteriography and CT during arterial portography" (PDF). Eur Radiol. 12 (3): 701–2. doi:10.1007/s003300101048. PMID 11870491.
- 1 2 3 Taylor AC, Palmer KR (February 1998). "Caroli's disease". Eur J Gastroenterol Hepatol. 10 (2): 105–8. doi:10.1097/00042737-199802000-00001. PMID 9581983.
- ↑ Ulrich F, Steinmüller T, Settmacher U, et al. (September 2002). "Therapy of Caroli's disease by orthotopic liver transplantation". Transplant. Proc. 34 (6): 2279–80. doi:10.1016/S0041-1345(02)03235-9. PMID 12270398.
- 1 2 Jacques Caroli at Who Named It?
- ↑ Miller WJ, Sechtin AG, Campbell WL, Pieters PC (1 August 1995). "Imaging findings in Caroli's disease". AJR Am J Roentgenol. 165 (2): 333–7. doi:10.2214/ajr.165.2.7618550. PMID 7618550.