Superior laryngeal nerve
| Superior laryngeal nerve | |
|---|---|
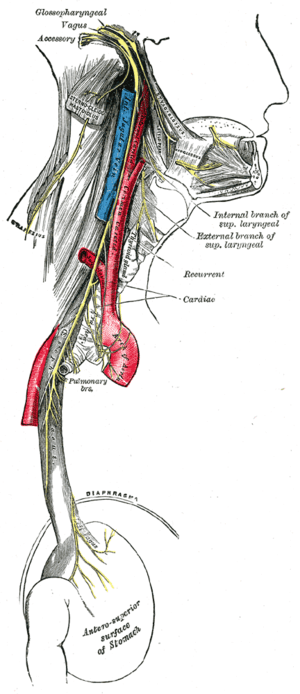
 Plan of upper portions of glossopharyngeal, vagus, and accessory nerves. ("Laryngeal" labeled at lower right.) | |
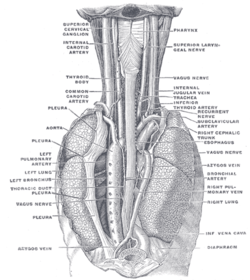
 Course and distribution of the glossopharyngeal, vagus, and accessory nerves. (Branches visible in upper right.) | |
| Details | |
| Innervates | larynx |
| Identifiers | |
| Latin | nervus laryngeus superior |
| TA | A14.2.01.160 |
| FMA | 6239 |
The superior laryngeal nerve is a branch of the vagus nerve. It arises from the middle of the inferior ganglion of vagus nerve and in its course receives a branch from the superior cervical ganglion of the sympathetic nervous system.
All intrinsic laryngeal muscles except the cricothyroids are innervated by the recurrent laryngeal nerve. The cricothyroid muscles are innervated by the superior laryngeal nerve.
The recurrent laryngeal nerve gets its name from the fact that it loops below the aorta on its way to the intrinsic muscles of the larynx. The left recurrent laryngeal nerve passes under and around the aorta on its way to the larynx, whereas the right recurrent laryngeal nerve passes under and around the subclavian artery. Because the aorta is inferior to the subclavian artery, the left recurrent laryngeal nerve is a bit longer than the right recurrent laryngeal nerve. However, there is no discernible effect on the timing of neural impulses to the muscles these two nerves serve. By comparison with the recurrent laryngeal nerves, the superior laryngeal nerve takes a more direct route on the way to the cricothyroid muscles.[1]
Structure
The superior laryngeal nerve descends, by the side of the pharynx, behind the internal carotid artery, and divides into two branches:
Pathology
A superior laryngeal nerve palsy changes the pitch of the voice and causes an inability to make explosive sounds due to paralysis of the cricothyroid muscle. If no recovery is evident three months after the palsy initially presents, the damage is most likely to be permanent. A bilateral palsy presents as a tiring and hoarse voice. It can be injured in surgery involving the removal of the thyroid gland (thyroidectomy).
Additional images
 The position and relation of the esophagus in the cervical region and in the posterior mediastinum. Seen from behind.
The position and relation of the esophagus in the cervical region and in the posterior mediastinum. Seen from behind.
References
- ↑ Fuller, D. R., Pimentel, J. T., & Peregoy, B. M. (2012). Applied anatomy & physiology for speech-language pathology & audiology. Baltimore, MD: Wolters Kluwer- Lippincott Williams & Wilkins.
This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
Fuller, D. R., Pimentel, J. T., & Peregoy, B. M. (2012). Applied anatomy & physiology for speech-language pathology & audiology. Baltimore, MD: Wolters Kluwer- Lippincott Williams & Wilkins.
External links
- -2066743236 at GPnotebook
- cranialnerves at The Anatomy Lesson by Wesley Norman (Georgetown University) (X)