Pancreatitis
| Pancreatitis | |
|---|---|
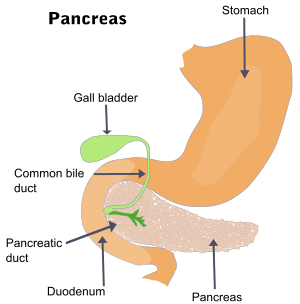 | |
| The pancreas and surrounding organs | |
| Classification and external resources | |
| Specialty | Gastroenterology, general surgery |
| ICD-10 | K85, K86.0–K86.1 |
| ICD-9-CM | 577.0–577.1 |
| OMIM | 167800 |
| DiseasesDB | 24092 |
| MedlinePlus | 001144 |
| eMedicine | emerg/354 |
| MeSH | D010195 |
| GeneReviews | |
Pancreatitis is inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes. There are two main types, acute pancreatitis and chronic pancreatitis. Signs and symptoms of pancreatitis include pain in the upper abdomen, nausea and vomiting. The pain often goes into the back and is usually severe. In acute pancreatitis a fever may occur and symptoms typically resolve in a few days. In chronic pancreatitis weight loss, fatty stool, and diarrhea may occur. Complications may include infection, bleeding, diabetes mellitus, or problems with other organs.[1]
The most common causes of acute pancreatitis are gallstones and heavy alcohol use. Other causes include direct trauma, certain medications, infections such as mumps, and tumors among others. Chronic pancreatitis may develop as a result of acute pancreatitis. It is most commonly due to many years of heavy alcohol use. Other causes include high levels of blood fats, high blood calcium, some medications, and certain genetic disorders such as cystic fibrosis among others.[1] Smoking increases the risk of both acute and chronic pancreatitis.[2][3] Diagnosis of acute pancreatitis is based on a threefold increase in the blood of either amylase or lipase. In chronic pancreatitis these tests may be normal. Medical imaging such as ultrasound and CT scan may also be useful.[1]
Acute pancreatitis is usually treated with intravenous fluids, pain medication, and sometimes antibiotics. Typically no eating or drinking is allowed and a tube may be placed into the stomach. A procedure known as an endoscopic retrograde cholangiopancreatography (ERCP) may be done to open the pancreatic duct if blocked. In those with gallstones the gallbladder is often also removed. In chronic pancreatitis, in addition to the above, temporary feeding through a nasogastric tube may be used to provide adequate nutrition. Long-term dietary changes and pancreatic enzyme replacement may be required. And occasionally surgery is done to remove parts of the pancreas.[1]
Globally, in 2013 about 17 million cases of pancreatitis occurred.[4] This resulted in 123,000 deaths, up from 83,000 deaths in 1990.[5] Acute pancreatitis occurs in about 30 per 100,000 people a year.[2] New cases of chronic pancreatitis develop in about 8 per 100,000 people a year and currently affect about 50 per 100,000 people in the United States.[6] It is more common in men than women. Often chronic pancreatitis starts between the ages of 30 and 40 while it is rare in children.[1] Acute pancreatitis was first described on autopsy in 1882 while chronic pancreatitis was first described in 1946.[6]
Signs and symptoms
The most common symptoms of pancreatitis are severe upper abdominal or left upper quadrant burning pain radiating to the back, nausea, and vomiting that is worse with eating. The physical examination will vary depending on severity and presence of internal bleeding. Blood pressure may be elevated by pain or decreased by dehydration or bleeding. Heart and respiratory rates are often elevated. The abdomen is usually tender but to a lesser degree than the pain itself. As is common in abdominal disease, bowel sounds may be reduced from reflex bowel paralysis. Fever or jaundice may be present. Chronic pancreatitis can lead to diabetes or pancreatic cancer. Unexplained weight loss may occur from a lack of pancreatic enzymes hindering digestion.
Causes
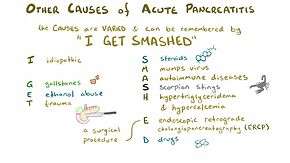
Eighty percent of cases of pancreatitis are caused by alcohol or gallstones. Gallstones are the single most common cause of acute pancreatitis.[7] Alcohol is the single most common cause of chronic pancreatitis.[8][9][10][11][12]
Some medications are commonly associated with pancreatitis, most commonly corticosteroids such as prednisolone, but also including the HIV drugs didanosine and pentamidine, diuretics, the anticonvulsant valproic acid, the chemotherapeutic agents L-asparaginase and azathioprine, estrogen by way of increased blood triglycerides,[13] and antihyperglycemic agents like metformin,[14] vildagliptin,[15] and sitagliptin.[16] It may be noted here that the drugs used to treat conditions that are themselves associated with increased events of pancreatitis may also be incidentally linked to pancreatitis. Examples include statins in dyslipidemia and gliptins in diabetes. According to the Food and Drug Administration's MedWatch Surveillance System and Published Reports Atypical, atypical antipsychotics such as clozapine, risperidone, and olanzapine can also be responsible for causing pancreatitis.[17]
Other common causes include trauma, mumps, autoimmune disease, high blood calcium, hypothermia, and endoscopic retrograde cholangiopancreatography (ERCP). Pancreas divisum is a common congenital malformation of the pancreas that may underlie some recurrent cases. Diabetes mellitus type 2 is associated with a 2.8-fold higher risk.[18]
Less common causes include pancreatic cancer, pancreatic duct stones,[19] vasculitis (inflammation of the small blood vessels in the pancreas), coxsackievirus infection, and porphyria—particularly acute intermittent porphyria and erythropoietic protoporphyria.
There is an inherited form that results in the activation of trypsinogen within the pancreas, leading to autodigestion. Involved genes may include Trypsin 1, which codes for trypsinogen, SPINK1, which codes for a trypsin inhibitor, or cystic fibrosis transmembrane conductance regulator.[20]
The mnemonic GETSMASHED is often used to remember the common causes of Pancreatitis: G—Gall stones E—Ethanol T—Trauma S—Steroids M—Mumps A—Autoimmune Pancreatitis S—Scorpion sting H—Hyperlipidaemia, Hypothermia, Hyperparathyroidism E—Endoscopic retrograde cholangiopancreatography D—Drugs commonly azathioprine, valproic acid
Infection
A number of infectious agents have been recognized as causes of pancreatitis including:[21]
Diagnosis

The differential diagnosis for pancreatitis includes but is not limited to cholecystitis, choledocholithiasis, perforated peptic ulcer, bowel infarction, small bowel obstruction, hepatitis and mesenteric ischemia .[22]
Diagnosis requires 2 of the 3 following criteria:
- Characteristic acute onset of epigastric or vague abdominal pain that may radiate to the back (see signs and symptoms above)
- Serum amylase or lipase levels > 3 times the upper limit of normal
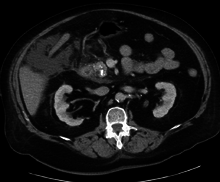
- An imaging study with characteristic changes. CT, MRI, abdominal ultrasound or endoscopic ultrasound can be used for diagnosis.
Amylase and lipase are 2 enzymes produced by the pancreas. Elevations in lipase are generally considered a better indicator for pancreatitis as it has greater specificity and has a longer half life.[23]
For imaging, abdominal ultrasound is convenient, simple, non-invasive, and inexpensive.[24] It is more sensitive and specific for pancreatitis from gallstones than other imaging modalities.[23] However, in 25–35% of patients the view of the pancreas can be obstructed by bowel gas making it difficult to evaluate.[22]
A contrast-enhanced CT scan is usually performed more than 48 hours after the onset of pain to evaluate for pancreatic necrosis and extrapancreatic fluid as well as predict the severity of the disease. CT scanning earlier can be falsely reassuring.
ERCP or an endoscopic ultrasound can also be used if a biliary cause for pancreatitis is suspected.
Treatment
The treatment of pancreatitis is supportive and depends on severity. Morphine generally is suitable for pain control. There are no clinical studies to suggest that morphine can aggravate or cause pancreatitis or cholecystitis.[25]
The treatment that is received for acute pancreatitis will depend on whether the diagnosis is for the mild form of the condition, which causes no complications, or the severe form, which can cause serious complications.
Mild acute pancreatitis
The treatment of mild acute pancreatitis is successfully carried out by admission to a general hospital ward. Traditionally, people were not allowed to eat until the inflammation resolved but more recent evidence suggests early feeding is safe and improves outcomes. Because pancreatitis can cause lung damage and affect normal lung function, oxygen is occasionally delivered through breathing tubes that are connected via the nose. The tubes can then be removed after a few days once it is clear that the condition is improving. Dehydration may result during an episode of acute pancreatitis, so fluids will be provided intravenously. The pain associated with even mild or moderate cases of acute pancreatitis can be severe, which means that a narcotic painkiller may be required.
Severe acute pancreatitis
Severe pancreatitis is associated with organ failure, necrosis, infected necrosis, pseudocyst, and abscess. If diagnosed with severe acute pancreatitis, people will need to be admitted to a high dependency unit or intensive care unit. It is likely that the levels of fluids inside the body will have dropped significantly as it diverts bodily fluids and nutrients in an attempt to repair the pancreas. The drop in fluid levels can lead to a reduction in the volume of blood within the body, which is known as hypovolemic shock. Hypovolemic shock can be life-threatening as it can very quickly starve the body of the oxygen-rich blood that it needs to survive. To avoid going into hypovolemic shock, fluids will be pumped intravenously. Oxygen will be supplied through tubes attached to the nose and ventilation equipment may be used to assist with breathing. Feeding tubes may be used to provide nutrients, combined with appropriate analgesia.
As with mild acute pancreatitis, it will be necessary to treat the underlying cause—gallstones, discontinuing medications, cessation of alcohol, etc. If the cause is gallstones, it is likely that an ERCP procedure or removal of the gallbladder will be recommended. The gallbladder should be removed during the same hospital admission or within two weeks of pancreatitis onset so as to limit the risk of recurrent pancreatitis. If the cause of pancreatitis is alcohol, cessation of alcohol consumption and treatment for alcohol dependency may improve pancreatitis. Even if the underlying cause is not related to alcohol consumption, doctors recommend avoiding it for at least six months as this can cause further damage to the pancreas during the recovery process.[26] Oral intake, especially fats, is generally restricted initially but early enteral feeding within 48 hours has been shown to improve clinical outcomes.[27] Fluids and electrolytes are replaced intravenously. Nutritional support is initiated via tube feeding to surpass the portion of the digestive tract most affected by secreted pancreatic enzymes if there is no improvement in the first 72–96 hours of treatment.[28]
Prognosis
Severe acute pancreatitis has mortality rates around 2–9%, higher where necrosis of the pancreas has occurred.[29]
Several scoring systems are used to predict the severity of an attack of pancreatitis. They each combine demographic and laboratory data to estimate severity or probability of death. Examples include APACHE II, Ranson, BISAP, and Glasgow. The Modified Glasgow criteria suggests that a case be considered severe if at least three of the following are true:[30]
- Age > 55 years
- Blood levels:
- PO2 Oxygen < 60mmHg or 7.9kPa
- White blood cells > 15
- Calcium < 2 mmol/L
- Urea > 16 mmol/L
- Lactate dehydrogenase (LDH) > 600iu/L
- Aspartate transaminase (AST) > 200iu/L
- Albumin < 32g/L
- Glucose > 10 mmol/L
This can be remembered using the mnemonic PANCREAS:
- PO2 Oxygen < 60mmHg or 7.9kPa
- Age > 55
- Neutrophilia White blood cells > 15
- Calcium < 2 mmol/L
- Renal Urea > 16 mmol/L
- Enzymes Lactate dehydrogenase (LDH) > 600iu/L Aspartate transaminase (AST) > 200iu/L
- Albumin < 32g/L
- Sugar Glucose > 10 mmol/L
The BISAP score (Blood urea nitrogen level >25 mg/dL, Impaired mental status, Systemic inflammatory response syndrome, age over 60 years, pleural effusion) has been validated as similar to other prognostic scoring systems.[31]
Complications
Early complications include shock, infection, systemic inflammatory response syndrome, low blood calcium, high blood glucose, and dehydration. Blood loss, dehydration, and fluid leaking into the abdominal cavity (ascites) can lead to kidney failure. Respiratory complications are often severe. Pleural effusion is usually present. Shallow breathing from pain can lead to lung collapse. Pancreatic enzymes may attack the lungs, causing inflammation. Severe inflammation can lead to intra-abdominal hypertension and abdominal compartment syndrome, further impairing renal and respiratory function and potentially requiring management with an open abdomen to relieve the pressure.[32]
Late complications include recurrent pancreatitis and the development of pancreatic pseudocysts—collections of pancreatic secretions that have been walled off by scar tissue. These may cause pain, become infected, rupture and bleed, block the bile duct and cause jaundice, or migrate around the abdomen. Acute necrotizing pancreatitis can lead to a pancreatic abscess, a collection of pus caused by necrosis, liquefaction, and infection. This happens in approximately 3% of cases, or almost 60% of cases involving more than two pseudocysts and gas in the pancreas.[33]
Epidemiology
Globally the incidence of acute pancreatitis is 5 to 35 cases per 100,000 people. The incidence of chronic pancreatitis is 4–8 per 100,000 with a prevalence of 26–42 cases per 100,000.[34] In 2013 pancreatitis resulted in 123,000 deaths up from 83,000 deaths in 1990.[5]
See also
References
- 1 2 3 4 5 "Pancreatitis". niddk.nih.gov. August 16, 2012. Retrieved 1 March 2015.
- 1 2 Lankisch, PG; Apte, M; Banks, PA (20 January 2015). "Acute pancreatitis.". Lancet. 386: 85–96. doi:10.1016/S0140-6736(14)60649-8. PMID 25616312.
- ↑ Yadav, D; Lowenfels, AB (June 2013). "The epidemiology of pancreatitis and pancreatic cancer.". Gastroenterology. 144 (6): 1252–61. doi:10.1053/j.gastro.2013.01.068. PMC 3662544
 . PMID 23622135.
. PMID 23622135. - ↑ Global Burden of Disease Study 2013, Collaborators (22 August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet (London, England). 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMID 26063472.
- 1 2 GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet. 385: 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604
 . PMID 25530442.
. PMID 25530442. - 1 2 Muniraj, T; Aslanian, HR; Farrell, J; Jamidar, PA (December 2014). "Chronic pancreatitis, a comprehensive review and update. Part I: epidemiology, etiology, risk factors, genetics, pathophysiology, and clinical features.". Disease-a-month : DM. 60 (12): 530–50. doi:10.1016/j.disamonth.2014.11.002. PMID 25510320.
- ↑ NIDDK (July 2008). "Pancreatitis". National Digestive Diseases Information Clearinghouse. U.S. National Institute of Diabetes and Digestive and Kidney Diseases. 08–1596.
- ↑ "Pancreatitis". A.D.A.M., Inc. Retrieved 2013-01-05.
- ↑ Apte MV, Pirola RC, Wilson JS (June 2009). "Pancreas: alcoholic pancreatitis—it's the alcohol, stupid". Nature Reviews Gastroenterology & Hepatology. 6 (6): 321–2. doi:10.1038/nrgastro.2009.84. PMID 19494819. Lay summary – Medscape Today.
- ↑ Yadav D, Hawes RH, Brand RE, Anderson MA, Money ME, Banks PA, Bishop MD, Baillie J, Sherman S, DiSario J, Burton FR, Gardner TB, Amann ST, Gelrud A, Lawrence C, Elinoff B, Greer JB, O'Connell M, Barmada MM, Slivka A, Whitcomb DC (June 2009). "Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis". Arch. Intern. Med. 169 (11): 1035–45. doi:10.1001/archinternmed.2009.125. PMID 19506173.
- ↑ "Pancreatitis Explained". Better Health Channel. State Government of Victoria. 2011.
- ↑ Johnson CD, Hosking S (1991). "National statistics for diet, alcohol consumption, and chronic pancreatitis in England and Wales, 1960–88". Gut. 32 (11): 1401–5. doi:10.1136/gut.32.11.1401. PMC 1379177
 . PMID 1752477.
. PMID 1752477. - ↑ Smith, Emma; Murray Longmore; Wilkinson, Ian; Tom Turmezei; Chee Kay Cheung (2007). Oxford handbook of clinical medicine (7th ed.). Oxford [Oxfordshire]: Oxford University Press. p. 584. ISBN 0-19-856837-1.
- ↑ Ben MH, Thabet H, Zaghdoudi I, Amamou M (2002). "Metformin associated acute pancreatitis". Veterinary and human toxicology. 44 (1): 47–48. PMID 11824780.
- ↑ Kunjathaya P, Ramaswami PK, Krishnamurthy AN, Bhat N (2013). "Acute necrotizing pancreatitis associated with vildagliptin". JOP : Journal of the pancreas. 14 (1): 81–84. doi:10.6092/1590-8577/1203. PMID 23306341.
- ↑ Matveyenko AV, Dry S, Cox HI, Moshtaghian A, Gurlo T, Galasso R, Butler AE, Butler PC (July 2009). "Beneficial endocrine but adverse exocrine effects of sitagliptin in the human islet amyloid polypeptide transgenic rat model of type 2 diabetes: interactions with metformin". Diabetes. 58 (7): 1604–15. doi:10.2337/db09-0058. PMC 2699878
 . PMID 19403868.
. PMID 19403868. - ↑ Koller EA, Cross JT, Doraiswamy PM, Malozowski SN (2003). "Pancreatitis Associated With Atypical Antipsychotics: From the Food and Drug Administration's MedWatch Surveillance System and Published Reports". Pharmacotherapy. 23 (9): 1123–30. doi:10.1592/phco.23.10.1123.32759. PMID 14524644.
- ↑ Noel RA, Braun DK, Patterson RE, Bloomgren GL (May 2009). "Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study". Diabetes Care. 32 (5): 834–8. doi:10.2337/dc08-1755. PMC 2671118
 . PMID 19208917.
. PMID 19208917. - ↑ Macaluso JN (August 1997). "Editorial Comment". J. Urol. 158 (2): 522. doi:10.1016/S0022-5347(01)64525-7. on Matthews K, Correa RJ, Gibbons RP, Weissman RM, Kozarek RA (August 1997). "Extracorporeal shock wave lithotripsy for obstructing pancreatic duct calculi". J. Urol. 158 (2): 522–5. doi:10.1016/s0022-5347(01)64524-5. PMID 9224338.
- ↑ D. Whitcomb (2006). "Genetic Testing for Pancreatitis".
- ↑ Parenti DM, Steinberg W, Kang P (November 1996). "Infectious causes of acute pancreatitis". Pancreas. 13 (4): 356–71. doi:10.1097/00006676-199611000-00005. PMID 8899796.
- 1 2 "Clinical manifestations and diagnosis of acute pancreatitis". www.uptodate.com. Retrieved 2015-12-08.
- 1 2 Hospitalist Handbook (4th ed.). Department of Medicine University of California, San Francisco. 2012. pp. 224–225.
- ↑ Lawrence W. Tierney; Stephen J. McPhee. Medicine. McGraw-Hill. ISBN 0-07-144441-6.
- ↑ Helm JF, Venu RP, Geenen JE, Hogan WJ, Dodds WJ, Toouli J, Arndorfer RC (October 1988). "Effects of morphine on the human sphincter of Oddi". Gut. 29 (10): 1402–7. doi:10.1136/gut.29.10.1402. PMC 1434014
 . PMID 3197985.
. PMID 3197985.
- ↑ E Medicine Health , Jerry R. Balentine, DO, FACEP , Melissa Conrad Stöppler, MD, Chief Medical Editor
- ↑ Li JY, Yu T, Chen GC, Yuan YH, Zhong W, Zhao LN, Chen QK (Jun 6, 2013). "Enteral Nutrition within 48 Hours of Admission Improves Clinical Outcomes of Acute Pancreatitis by Reducing Complications: A Meta-Analysis.". PLOS ONE. 8 (6): e64926. doi:10.1371/journal.pone.0064926. PMC 3675100
 . PMID 23762266.
. PMID 23762266. - ↑ Muddana V, Whitcomb DC, Papachristou GI (August 2009). "Current management and novel insights in acute pancreatitis". Expert Rev Gastroenterol Hepatol. 3 (4): 435–44. doi:10.1586/egh.09.27. PMID 19673630.
- ↑ Munoz A, Katerndahl DA (July 2000). "Diagnosis and management of acute pancreatitis". Am Fam Physician. 62 (1): 164–74. PMID 10905786.
- ↑ Corfield AP, Cooper MJ, Williamson RC, Mayer AD, McMahon MJ, Dickson AP, Shearer MG, Imrie CW (1985). "Prediction of severity in acute pancreatitis: prospective comparison of three prognostic indices". Lancet. 2 (8452): 403–7. doi:10.1016/S0140-6736(85)92733-3. PMID 2863441.
- ↑ Papachristou GI, Muddana V, Yadav D, O'Connell M, Sanders MK, Slivka A, Whitcomb DC (Feb 2010). "Comparison of BISAP, Ranson's, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis.". Am J Gastroenterol. 105 (2): 435–41. doi:10.1038/ajg.2009.622. PMID 19861954.
- ↑ Fitzgerald JE, Gupta S, Masterson S, Sigurdsson HH (April 2012). "Laparostomy management using the ABThera™ open abdomen negative pressure therapy system in a grade IV open abdomen secondary to acute pancreatitis". Int Wound J. 10 (2): 138–144. doi:10.1111/j.1742-481X.2012.00953.x. PMID 22487377.
- ↑ Pancreatic abscess at eMedicine
- ↑ Harrison's Principles of Internal Medicine. p. Chapter 370 Approach to the Patient with Pancreatic Disease. ISBN 978-0-07-1802161.
External links
| Wikimedia Commons has media related to Pancreatitis. |
- Pancreatitis at DMOZ
- Banks et al. modified Marshall Scoring System for Organ Dysfunction
- GeneReviews/NCBI/NIH/UW entry on PRSS1-Related Hereditary Pancreatitis