Fluorouracil
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌflʊroʊˈjʊrəˌsɪl/[1] |
| Trade names | Adrucil, Carac, Efudex, Efudix |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682708 |
| License data |
|
| Pregnancy category | |
| Routes of administration | IV (infusion or bolus) and topical |
| ATC code | L01BC02 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 28 to 100% |
| Protein binding | 8 to 12% |
| Metabolism | Intracellular and hepatic (CYP-mediated) |
| Biological half-life | 16 minutes |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number |
51-21-8 |
| PubChem (CID) | 3385 |
| IUPHAR/BPS | 4789 |
| DrugBank |
DB00544 |
| ChemSpider |
3268 |
| UNII |
U3P01618RT |
| KEGG |
D00584 |
| ChEBI |
CHEBI:46345 |
| ChEMBL |
CHEMBL185 |
| ECHA InfoCard | 100.000.078 |
| Chemical and physical data | |
| Formula | C4H3FN2O2 |
| Molar mass | 130.077 g/mol |
| 3D model (Jmol) | Interactive image |
| Melting point | 282–283 °C (540–541 °F) |
| |
| |
| (verify) | |
Fluorouracil (5-FU) (trade name Adrucil among others) is a medication which is used in the treatment of cancer.
It is a suicide inhibitor and works through irreversible inhibition of thymidylate synthase. It belongs to the family of drugs called the antimetabolites.[2] It is also a pyrimidine analog .
It is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.[3]
Medical uses
Fluorouracil has been given systemically for anal, breast, colorectal, oesophageal, stomach, pancreatic and skin cancers (especially head and neck cancers).[4] It has also been given topically (on the skin) for actinic keratoses, skin cancers and Bowen's disease[4] and as eye drops for treatment of ocular surface squamous neoplasia.[5]
Contraindications
It is contraindicated in patients that are severely debilitated or in patients with bone marrow suppression due to either radiotherapy or chemotherapy.[6] It is likewise contraindicated in pregnant or breastfeeding women.[6] It should also be avoided in patients that do not have malignant illnesses.[6]
Adverse effects
Adverse effects by frequency include:[4][6][7][8][9][10][11][12][13]
During systemic use
Common (> 1% frequency):
- Nausea
- Vomiting
- Diarrhea (see below for details)
- Mucositis
- Headache
- Myelosuppression (see below for details)
- Alopecia (hair loss)
- Photosensitivity
- Hand-foot syndrome
- Maculopapular eruption
- Itch
- Cardiotoxicity (see below for details)
- Persistent hiccups
- Mood disorders (irritability, anxiety, depression)
Uncommon (0.1–1% frequency):
- Oesophagitis
- GI ulceration and bleeding
- Proctitis
- Nail disorders
- Vein pigmentation
- Confusion
- Cerebellar syndrome
- Encephalopathy
- Visual changes
- Photophobia
- Lacrimation (the expulsion of tears without any emotional or physiologic reason)
Rare (< 0.1% frequency):
- Anaphylaxis
- Allergic reactions
- Fever without signs of infection
Diarrhea is severe and may be dose-limiting and is exacerbated by co-treatment with calcium folinate.[4] Neutropenia tends to peak about 9–14 days after beginning treatment.[4] Thrombocytopenia tends to peak about 7–17 days after the beginning of treatment and tends to recover about 10 days after its peak.[4] Cardiotoxicity is a fairly common side effect, but usually this cardiotoxicity is just angina or symptoms associated with coronary artery spasm, but in about 0.55% of those receiving the drug will develop life-threatening cardiotoxicity. Life-threatening cardiotoxicity includes: arrhythmias, ventricular tachycardia and cardiac arrest, secondary to transmural ischaemia.
During topical use
Common (> 1% frequency):
- Local pain
- Itchiness
- Burning
- Stinging
- Crusting
- Weeping
- Dermatitis
- Photosensitivity
Uncommon (0.1–1% frequency):
- hyper- or hypopigmentation
- Scarring
Neurological damage
5-FU injection and topical even in small doses cause both acute central nervous system (CNS) damage and progressively worsening delayed degeneration of the CNS in mice. This latter effect is caused by 5-FU-induced damage to the oligodendrocytes that produce the insulating myelin sheaths. [14] [15]
The United States package insert warns that acute cerebellar syndrome has been observed following injection of fluorouracil and may persist after cessation of treatment. Symptoms include Ataxia, nystagmus, and dysmetria.[16]
Potential overdose
There is very little difference between the minimum effective dose and maximum tolerated dose of 5-FU, and the drug exhibits marked individual pharmacokinetic variability.[17][18][19] Therefore, an identical dose of 5-FU may result in a therapeutic response with acceptable toxicity in some patients and unacceptable and possibly life-threatening toxicity in others.[17] Both overdosing and underdosing are of concern with 5-FU, although several studies have shown that the majority of colorectal cancer patients treated with 5-FU are underdosed based on today's dosing standard, body surface area (BSA).[20][21][22][23] The limitations of BSA-based dosing prevent oncologists from being able to accurately titer the dosage of 5-FU for the majority of individual patients, which results in sub-optimal treatment efficacy or excessive toxicity.[20][21]
Numerous studies have found significant relationships between concentrations of 5-FU in blood plasma and both desirable or undesirable effects on patients.[24][25] Studies have also shown that dosing based on the concentration of 5-FU in plasma can greatly increase desirable outcomes while minimizing negative side effects of 5-FU therapy.[20][26] One such test that has been shown to successfully monitor 5-FU plasma levels and which "may contribute to improved efficacy and safety of commonly used 5-FU-based chemotherapies" is the My5-FU test.[22][27][28]
Interactions
Its use should be avoided in patients receiving drugs known to modulate dihydropyrimidine dehydrogenase (such as the antiviral drug sorivudine).[6] It may also increase the INR and prothrombin times in patients on warfarin.[6] Fluoruracil's efficacy is decreased when used alongside allopurinol which can be used to decrease fluoruracil induced stomatitis through use of allopurinol mouthwash.[29]
Pharmacology
Pharmacogenetics
The dihydropyrimidine dehydrogenase (DPD) enzyme is responsible for the detoxifying metabolism of fluoropyrimidines, a class of drugs that includes 5-fluorouracil, capecitabine, and tegafur.[30] Genetic variations within the DPD gene (DPYD) can lead to reduced or absent DPD activity, and individuals who are heterozygous or homozygous for these variations may have partial or complete DPD deficiency; an estimated 0.2% of individuals have complete DPD deficiency.[30][31] Those with partial or complete DPD deficiency have a significantly increased risk of severe or even fatal drug toxicities when treated with fluoropyrimidines; examples of toxicities include myelosuppression, neurotoxicity and hand-foot syndrome.[30][31]
Mechanism of action
5-FU acts in several ways, but principally as a thymidylate synthase (TS) inhibitor. Interrupting the action of this enzyme blocks synthesis of the pyrimidine thymidine, which is a nucleoside required for DNA replication. Thymidylate synthase methylates deoxyuridine monophosphate (dUMP) to form thymidine monophosphate (dTMP). Administration of 5-FU causes a scarcity in dTMP, so rapidly dividing cancerous cells undergo cell death via thymineless death.[32] Calcium folinate provides an exogenous source of reduced folinates and hence stabilises the 5-FU-TS complex, hence enhancing 5-FU's cytotoxicity.[33]
History
In 1954 Abraham Cantarow and Karl Paschkis found liver tumors absorbed radioactive uracil more readily than normal liver cells. Charles Heidelberger, who had earlier found that fluorine in fluoroacetic acid inhibited a vital enzyme, asked Robert Duschinsky and Robert Schnitzer at Hoffman-La Roche to synthesize fluorouracil.[34] Some credit Heidelberger and Duschinsky with the discovery that 5-fluorouracil markedly inhibited tumors in mice.[35] The original 1957 report[36][37] in Nature has Heidelberger as lead author, along with N. K. Chaudhuri, Peter Danneberg, Dorothy Mooren, Louis Griesbach, Robert Duschinsky, R. J. Schnitzer, E. Pleven, and J. Scheiner.[38]
Natural analogues
In 2003 it was discovered that a closely related compound is produced by a marine sponge, Phakellia fusca. This is significant because fluorine-containing organic compounds exist only rarely in nature, and also because manmade anticancer drugs are not frequently found to have analogues in nature.[39]
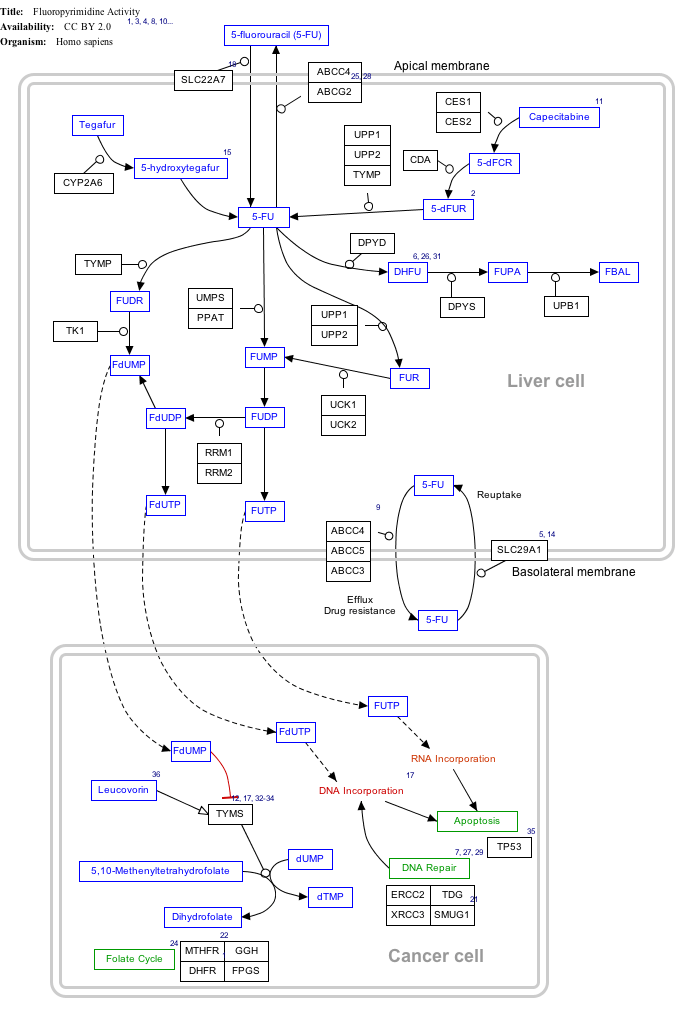
Interactive pathway map
Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
Fluorouracil (5-FU) Activity edit
- ↑ The interactive pathway map can be edited at WikiPathways: "FluoropyrimidineActivity_WP1601".
Names
The name "fluorouracil" is the INN, USAN, USP name, and BAN. The form "5-fluorouracil" is often used; it shows that there is a fluorine atom on the 5th carbon of a uracil ring.
References
- ↑ "Fluorouracil - Definition and More from the Free Merriam-Webster Dictionary". Retrieved 2014-11-19.
- ↑ Brayfield, A., ed. (13 December 2013). "Fluorouracil". Martindale: The Complete Drug Reference. Pharmaceutical Press. Retrieved 16 April 2014.
- ↑ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- 1 2 3 4 5 6 7 Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- ↑ Joag, Madhura G.; Sise, Adam; Murillo, Juan Carlos; Sayed-Ahmed, Ibrahim Osama; Wong, James R.; Mercado, Carolina; Galor, Anat; Karp, Carol L. (2016-03-27). "Topical 5-Fluorouracil 1% as Primary Treatment for Ocular Surface Squamous Neoplasia". Ophthalmology. doi:10.1016/j.ophtha.2016.02.034. ISSN 1549-4713. PMID 27030104.
- 1 2 3 4 5 6 "Fluorouracil 50 mg/ml Injection - Summary of Product Characteristics". electronic Medicines Compendium. Hospira UK Ltd. 24 August 2011. Retrieved 24 January 2014.
- ↑ "DBL Fluorouracil Injection BP" (PDF). TGA eBusiness Services. Hospira Australia Pty Ltd. 21 June 2012. Retrieved 24 January 2014.
- ↑ "ADRUCIL (fluorouracil) injection [Teva Parenteral Medicines, Inc.]". DailyMed. Teva Parenteral Medicines, Inc. August 2012. Retrieved 24 January 2014.
- 1 2 "Efudex, Carac (fluorouracil topical) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Retrieved 24 January 2014.
- ↑ "Adrucil (fluorouracil) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Retrieved 24 January 2014.
- ↑ Ha, JH; Hwang, DY; Yu, J; Park, DH; Ryu, SH (2011). "Onset of Manic Episode during Chemotherapy with 5-Fluorouracil". Psychiatry Investig. 8: 71–3. doi:10.4306/pi.2011.8.1.71. PMC 3079190
 . PMID 21519541.
. PMID 21519541. - ↑ Park H. J., Choi Y. T., Kim I. H., Hah J. C.; A case of reversible dementia associated with depression in a patient on 5-FU or its analogue drugs. J. Korean Neuropsychiatr. Assoc. 1987;30:199–202.
- ↑ MedsFacts meta-analysis covering adverse side effect reports of 5fu(fluorouracil) patients who developed hiccups at MedsFact, 2013
- ↑ "Researchers Detail Chemotherapy's Damage to the Brain".
- ↑ "Common Cancer Treatments Toxic to Healthy Brain Cells".
- ↑ "Adrucil (Fluorouracil) Injection [TEVA Parenteral Medicines, Inc.]".
- 1 2 Gamelin, E.; Boisdron-Celle, M. (1999). "Dose monitoring of 5-fluorouracil in patients with colorectal or head and neck cancer—status of the art". Critical Reviews in Oncology/Hematology. 30 (1): 71–79. doi:10.1016/s1040-8428(98)00036-5.
- ↑ Felici A.; J. Verweij; Sparreboom A. (2002). "Dosing strategies for anticancer drugs: the good, the bad and body-surface area". Eur J Cancer. 38 (13): 1677–84. doi:10.1016/s0959-8049(02)00151-x.
- ↑ Baker S. D.; Verweij J.; Rowinsky E. K.; Donehower R. C.; Schellens J. H.; Grochow L. B.; Sparreboom A. (2002). "Role of body surface area in dosing of investigational anticancer agents in adults, 1991-2001". J. Natl Cancer Inst. 94 (24): 1883–8. doi:10.1093/jnci/94.24.1883.
- 1 2 3 Capitain O.; Asevoaia A.; Boisdron-Celle M.; Poirier A. L.; Morel A.; Gamelin E. (2012). "Individual Fluorouracil Dose Adjustment in FOLFOX Based on Pharmacokinetic Follow-Up Compared With Conventional Body-Area-Surface Dosing: A Phase II, Proof-of-Concept Study". Clin. Colorectal Cancer. 11 (4): 263–267. doi:10.1016/j.clcc.2012.05.004.
- 1 2 Saam, J; Critchfield G. C.; Hamilton S. A.; Roa B. B.; Wenstrup R. J.; Kaldate R. R. (2011). "Body surface area-based dosing of 5-fluoruracil results in extensive interindividual variability in 5-fluorouracil exposure in colorectal cancer patients on FOLFOX regimens". Clin Colorectal Cancer. 10 (3): 203–6. doi:10.1016/j.clcc.2011.03.015.
- 1 2 Beumer J. H.; Boisdron-Celle M.; Clarke W.; Courtney J. B.; Egorin M. J.; Gamelin E; Harney R. L.; Hammett-Stabler C; Lepp S.; Li Y.; Lundell G. D.; McMillin G.; Milano G.; Salamone S. J. (2009). "Multicenter evaluation of a novel nanoparticle immunoassay for 5-fluorouracil on the Olympus AU400 analyzer". Ther. Drug Monit. 31 (6): 688–94.
- ↑ Goldberg R. M.; Rothenberg M. L.; Van Cutsem E.; Benson A. B. 3rd; Blanke C. D.; Diasio R. B.; Grothey A.; Lenz H. J.; Meropol N. J.; Ramanathan R. K.; Becerra C. H.; Wickham R.; Armstrong D.; Viele C. (2007). "The Continuum of Care: A Paradigm for the Management of Metastatic Colorectal Cancer". The Oncologist. 12: 38–50. doi:10.1634/theoncologist.12-1-38.
- ↑ Ploylearmsaeng, S.-a.; Fuhr U.; Jetter A. (2006). "How may Anticancer Chemotherapy with Fluorouracil be Individualised?". Clin Pharmacokinet. 45 (6): 567–92. doi:10.2165/00003088-200645060-00002.
- ↑ van Kuilenburg, A. B.; Maring J. G. (2013). "Evaluation of 5-fluorouracil pharmacokinetic models and therapeutic drug monitoring in cancer patients". Pharmacogenomics. 14 (7): 799–811. doi:10.2217/pgs.13.54.
- ↑ Gamelin E. C.; Delva R.; Jacob J.; Merrouche Y; Raoul J. L.; Pezet D.; Dorval E.; Piot G.; Morel A.; Boisdron-Celle M. (2008). "Individual fluorouracil dose adjustment based on pharmacokinetic follow-up compared with conventional dosage: Results of a multicenter randomized trial of patients with metastatic colorectal cancer". J. Clin. Oncol. 26 (13): 2099–2105. doi:10.1200/jco.2007.13.3934.
- ↑ "Customizing Chemotherapy for Better Cancer Care". MyCare Diagnostics.
- ↑ "A Brief History of BSA Dosing". MyCare Diagnostics.
- ↑ Porta C, Moroni M, Nastasi G (1994). "Allopurinol mouthwashes in the treatment of 5-fluorouracil-induced stomatitis". Am. J. Clin. Oncol. 17 (3): 246–7. doi:10.1097/00000421-199406000-00014. PMID 8192112.
- 1 2 3 Caudle, KE; Thorn, CF; Klein, TE; Swen, JJ; McLeod, HL; Diasio, RB; Schwab, M (December 2013). "Clinical Pharmacogenetics Implementation Consortium guidelines for dihydropyrimidine dehydrogenase genotype and fluoropyrimidine dosing.". Clinical pharmacology and therapeutics. 94 (6): 640–5. doi:10.1038/clpt.2013.172. PMID 23988873.
- 1 2 Amstutz, U; Froehlich, TK; Largiadèr, CR (September 2011). "Dihydropyrimidine dehydrogenase gene as a major predictor of severe 5-fluorouracil toxicity.". Pharmacogenomics. 12 (9): 1321–36. doi:10.2217/pgs.11.72. PMID 21919607.
- ↑ Longley D. B.; Harkin D. P.; Johnston P. G. (May 2003). "5-fluorouracil: mechanisms of action and clinical strategies". Nat. Rev. Cancer. 3 (5): 330–8. doi:10.1038/nrc1074. PMID 12724731.
- ↑ Álvarez, P.; Marchal, J. A.; Boulaiz, H.; Carrillo, E.; Vélez, C.; Rodríguez-Serrano, F.; Melguizo, C.; Prados, J.; Madeddu, R.; Aranega, A. (February 2012). "5-Fluorouracil derivatives: a patent review". Expert Opinion on Therapeutic Patents. 22 (2): 107–123. doi:10.1517/13543776.2012.661413. PMID 22329541.
- ↑ Sneader W. (2005). Drug Discovery, p. 255.
- ↑ Cohen, Seymour (30 January 2008). "50 years ago in cell biology: A virologist recalls his work on cell growth inhibition". The Scientist.
- ↑ Chu E (September 2007). "Ode to 5-Fluorouracil". Clinical Colorectal Cancer. 6 (9): 609. doi:10.3816/CCC.2007.n.029.
- ↑ National Academy of Sciences, Biographical Memoirs,80:135
- ↑ Heidelberger C.; Chaudhuri N. K.; Danneberg P.; et al. (March 1957). "Fluorinated pyrimidines, a new class of tumour-inhibitory compounds". Nature. 179 (4561): 663–6. doi:10.1038/179663a0. PMID 13418758.
- ↑ Xu, Xiao-Hua; Yao, Guang-Min; Li, Yan-Ming; Lu, Jian-Hua; Lin, Chang-Jiang; Wang, Xin; Kong, Chui-Hua (2003-02-01). "5-Fluorouracil derivatives from the sponge Phakellia fusca". Journal of Natural Products. 66 (2): 285–288. doi:10.1021/np020034f. ISSN 0163-3864. PMID 12608868.