Carbamazepine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Tegretol |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682237 |
| License data | |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | N03AF01 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ~100%[1] |
| Protein binding | 70-80%[1] |
| Metabolism | Hepatic—by CYP3A4, to active epoxide form (carbamazepine-10,11 epoxide)[1] |
| Biological half-life | 36 hours (single dose), 16-24 hours (repeated dosing)[1] |
| Excretion | Urine (72%), feces (28%)[1] |
| Identifiers | |
| |
| CAS Number |
298-46-4 |
| PubChem (CID) | 2554 |
| IUPHAR/BPS | 5339 |
| DrugBank |
DB00564 |
| ChemSpider |
2457 |
| UNII |
33CM23913M |
| KEGG |
D00252 |
| ChEBI |
CHEBI:3387 |
| ChEMBL |
CHEMBL108 |
| Chemical and physical data | |
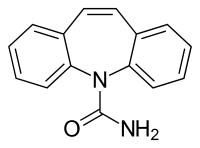
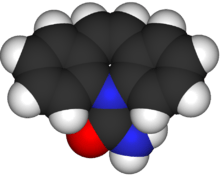
| Formula | C15H12N2O |
| Molar mass | 236.269 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Carbamazepine (CBZ), sold under the tradename Tegretol among others, is a medication used primarily in the treatment of epilepsy and neuropathic pain.[2] For seizures it works as well as phenytoin and valproate.[3][4] It is not effective for absence seizures or myoclonic seizures. It may be used in schizophrenia along with other medications and as a second line agent in bipolar disorder.[2] It is taken two to four times per day.[2] A controlled release formulation is available for which there is tentative evidence showing fewer side effects.[5]
Common side effects include nausea and drowsiness. Serious side effects may include skin rashes, decreased bone marrow function, suicidal thoughts, or confusion. It should not be used in those with a history of bone marrow problems. Use during pregnancy may cause harm to the baby; however stopping it in pregnant women with seizures is not recommended. Its use during breastfeeding is not recommended. Care should be taken in those with either kidney or liver problems.[2]
Carbamazepine was discovered in 1953 by Swiss chemist Walter Schindler.[6] It was first marketed in 1962.[7] It is available as a generic medication and is not very expensive.[8] It is on the WHO Model List of Essential Medicines, the most important medications needed in a basic health system.[9] The wholesale cost in the developing world is between 0.01 and 0.07 USD per dose as of 2014.[10]
Medical uses

Carbamazepine is typically used for the treatment of seizure disorders and neuropathic pain.[2] It is used off-label as a second-line treatment for bipolar disorder and in combination with an antipsychotic in some cases of schizophrenia when treatment with a conventional antipsychotic alone has failed.[2][11]
In the United States, the FDA-approved medical uses are epilepsy (including partial seizures, generalized tonic-clonic seizures and mixed seizures), trigeminal neuralgia, and manic and mixed episodes of bipolar I disorder.[12]
It is unclear if there is a significant difference in effectiveness between controlled release and immediate release formulations in epilepsy.[13] Controlled release forms might, however, have lower risks of side effects.[13]
Adverse effects
In the US, the label for carbamazepine contains warnings concerning:
- effects on the body's production of red blood cells, white blood cells, and platelets: rarely, there are major effects of aplastic anemia and agranulocytosis reported and more commonly, there are minor changes such as decreased white blood cell or platelet counts, that do not progress to more serious problems.[1]
- increased risks of suicide[1]
- risk of seizures, if the person stops taking the drug abruptly[1]
- risks to the fetus in women who are pregnant, specifically congenital malformations like spina bifida, and developmental disorders.[1][14]
Common adverse effects may include drowsiness, dizziness, headaches and migraines, motor coordination impairment, nausea, vomiting, and/or constipation. Alcohol use while taking carbamazepine may lead to enhanced depression of the central nervous system.[1] Less common side effects may include increased risk of seizures in people with mixed seizure disorders,[15] abnormal heart rhythms, blurry or double vision.[1] Also, rare case reports of an auditory side effect have been made, whereby patients perceive sounds about a semitone lower than previously; this unusual side effect is usually not noticed by most people, and disappears after the person stops taking carbamazepine.[16]
Interactions
Carbamazepine has a potential for drug interactions; caution should be used in combining other medicines with it, including other antiepileptics and mood stabilizers.[12] Lower levels of carbamazepine are seen when administrated with phenobarbital, phenytoin, or primidone, which can result in breakthrough seizure activity. Carbamazepine, as a CYP450 inducer, may increase clearance of many drugs, decreasing their concentration in the blood to subtherapeutic levels and reducing their desired effects.[17] Drugs that are more rapidly metabolized with carbamazepine include warfarin, lamotrigine, phenytoin, theophylline, and valproic acid.[12] Drugs that decrease the metabolism of carbamazepine or otherwise increase its levels include erythromycin,[18] cimetidine, propoxyphene, and calcium channel blockers.[12] Carbamazepine also increases the metabolism of the hormones in birth control pills and can reduce their effectiveness, potentially leading to unexpected pregnancies.[12] As a drug that induces cytochrome P450 enzymes, it accelerates elimination of many benzodiazepines and decreases their action.[19]
Valproic acid and valnoctamide both inhibit microsomal epoxide hydrolase (MEH), the enzyme responsible for the breakdown of carbamazepine-10,11 epoxide into inactive metabolites.[20] By inhibiting MEH, valproic acid and valnoctamide cause a build-up of the active metabolite, prolonging the effects of carbamazepine and delaying its excretion.
Grapefruit juice raises the bioavailability of carbamazepine by inhibiting CYP3A4 enzymes in the gut wall and in the liver.[1] Carbamazepine increases the processing of methadone resulting in lower blood levels.[21]
Pharmacogenetics
Dangerous and potentially fatal skin reactions, including Stevens–Johnson syndrome and toxic epidermal necrolysis, caused by carbamazepine therapy are significantly more common in patients with a particular human leukocyte antigen allele, HLA-B*1502.[22] Odds ratios for the development of Stevens-Johnson syndrome or toxic epidermal necrolysis in patients who carry the allele can be in the double, triple or even quadruple digits, depending on the population studied.[23][24] HLA-B*1502 occurs almost exclusively in patients with ancestry across broad areas of Asia, but has a very low or absent frequency in European, Japanese, Korean and African populations.[22][25] However, the HLA-A*31:01 allele has been shown to be a strong predictor of both mild and severe adverse reactions to carbamazepine among Japanese and Europeans.[24]
Pharmacokinetics
Carbamazepine is relatively slowly but well absorbed after oral administration. Its plasma half-life is about 30 hours when it is given as single dose, but it is a strong inducer of hepatic enzymes and the plasma half-life shortens to about 15 hours when it is given repeatedly.
Mechanism of action
The mechanism of action of carbamazepine and its derivatives is relatively well understood. Carbamazepine is a use-dependant blocker of voltage-gated sodium channels. It is ionised within intracellular fluid, and is then able to bind to activated voltage-gated sodium channels, preventing repetitive and sustained firing of an action potential.This leaves the affected cells less excitable until the drug dissociates. Carbamazepine is also a GABA receptor agonist, as it has also been shown to potentiate GABA receptors made up of alpha1, beta2, and gamma2 subunits.[26] This mechanism may contribute to its efficacy in neuropathic pain and bipolar disorder. Laboratory research has further demonstrated that carbamazepine is a serotonin releasing agent and possibly even a serotonin reuptake inhibitor.[27][28][29]
History
Carbamazepine was discovered by chemist Walter Schindler at J.R. Geigy AG (now part of Novartis) in Basel, Switzerland, in 1953.[30][31] It was first marketed as a drug to treat epilepsy in Switzerland in 1963 under the brand name "Tegretol"; its use for trigeminal neuralgia (formerly known as tic douloureux) was introduced at the same time.[30] It has been used as an anticonvulsant and antiepileptic in the UK since 1965, and has been approved in the US since 1968.[2]
In 1971, Drs. Takezaki and Hanaoka first used carbamazepine to control mania in patients refractory to antipsychotics (lithium was not available in Japan at that time). Dr. Okuma, working independently, did the same thing with success. As they were also epileptologists, they had some familiarity with the antiaggression effects of this drug. Carbamazepine was studied for bipolar disorder throughout the 1970s.[32]
Environmental fate
Carbamazepine has been detected in wastewater effluent.[33]:224 Field and laboratory studies have been conducted to understand the accumulation of carbamazepine in food plants grown in soil treated with sludge, which vary with respect to the concentrations of carbamazepine present in sludge and in the concentrations of sludge in the soil; taking into account only studies that used concentrations normally found, a 2014 review found that "the accumulation of carbamazepine into plants grown in soil amended with biosolids poses a de minimis risk to human health according to the approach."[33]:227
Brand names
Carbamazepine is available worldwide under many brand names.[34]
See also
- Imipramine
- Oxcarbazepine
- Toll-like receptor 4 investigating agonist (proinflammatory) property
References
- 1 2 3 4 5 6 7 8 9 10 11 12 "Carbamazepine Drug Label".
- 1 2 3 4 5 6 7 "Carbamazepine". The American Society of Health-System Pharmacists. Retrieved Mar 2015. Check date values in:
|access-date=(help) - ↑ Nolan, SJ; Marson, AG; Weston, J; Tudur Smith, C (28 April 2016). "Phenytoin versus valproate monotherapy for partial onset seizures and generalised onset tonic-clonic seizures: an individual participant data review.". The Cochrane database of systematic reviews. 4: CD001769. PMID 27123830.
- ↑ Nolan, SJ; Marson, AG; Weston, J; Tudur Smith, C (14 August 2015). "Carbamazepine versus phenytoin monotherapy for epilepsy: an individual participant data review.". The Cochrane database of systematic reviews (8): CD001911. PMID 26275105.
- ↑ Powell, G; Saunders, M; Rigby, A; Marson, AG (3 December 2014). "Immediate-release versus controlled-release carbamazepine in the treatment of epilepsy.". The Cochrane database of systematic reviews (12): CD007124. PMID 25470302.
- ↑ Smith, Howard S. (2009). Current therapy in pain. Philadelphia: Saunders/Elsevier. p. 460. ISBN 9781416048367.
- ↑ Moshé, Solomon (2009). The treatment of epilepsy (3 ed.). Chichester, UK: Wiley-Blackwell. p. xxix. ISBN 9781444316674.
- ↑ Principles and practice of stereotactic radiosurgery. New York: Springer. 2008. p. 536. ISBN 9780387710709.
- ↑ "WHO Model List of Essential Medicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ↑ "Carbamazepine". International Drug Price Indicator Guide. Retrieved 2 December 2015.
- ↑ Ceron-Litvoc D, Soares BG, Geddes J, Litvoc J, de Lima MS (January 2009). "Comparison of carbamazepine and lithium in treatment of bipolar disorder: a systematic review of randomized controlled trials". Hum Psychopharmacol. 24 (1): 19–28. doi:10.1002/hup.990. PMID 19053079.
- 1 2 3 4 5 Lexi-Comp (February 2009). "Carbamazepine". The Merck Manual Professional. Archived from the original on 2010-11-18. Retrieved on May 3, 2009.
- 1 2 Powell, G; Saunders, M; Rigby, A; Marson, AG (3 December 2014). "Immediate-release versus controlled-release carbamazepine in the treatment of epilepsy.". The Cochrane database of systematic reviews. 12: CD007124. doi:10.1002/14651858.CD007124.pub4. PMID 25470302.
- ↑ Jentink, J; Dolk, H; Loane, MA; Morris, JK; Wellesley, D; Garne, E; de Jong-van den Berg, L; EUROCAT Antiepileptic Study Working Group (2010-12-02). "Intrauterine exposure to carbamazepine and specific congenital malformations: systematic review and case-control study". BMJ (Clinical research ed.). 341: c6581. doi:10.1136/bmj.c6581. PMC 2996546
 . PMID 21127116.
. PMID 21127116. - ↑ Lige Liu; Thomas Zheng; Margaret J. Morris; Charlott Wallengren; Alison L. Clarke; Christopher A. Reid; Steven Petrou; Terence J. O'Brien (2006). "The Mechanism of Carbamazepine Aggravation of Absence Seizures". JPET. 319 (2): 790–798. doi:10.1124/jpet.106.104968. PMID 16895979.
- ↑ "Carbamazepine-induced transient auditory pitch-perception deficit.". Pediatr Neurol. 35: 131–4. Aug 2006. doi:10.1016/j.pediatrneurol.2006.01.011. PMID 16876011.
- ↑ "eMedicine - Toxicity, Carbamazepine". Archived from the original on 2008-08-04.
- ↑ Stafstrom CE, Nohria V, Loganbill H, Nahouraii R, Boustany RM, DeLong GR (January 1995). "Erythromycin-induced carbamazepine toxicity: a continuing problem". Arch Pediatr Adolesc Med. 149 (1): 99–101. doi:10.1001/archpedi.1995.02170130101025. PMID 7827672. Archived from the original on 2010-11-18.
- ↑ Moody D (2004). "Drug interactions with benzodiazepines". In Raymon LP, Mozayani A. Handbook of Drug Interactions: a Clinical and Forensic Guide. Humana. pp. 3–88. ISBN 1-58829-211-8.
- ↑ Gonzalez, Frank J.; Robert H. Tukey (2006). "Drug Metabolism". In Laurence Brunton; John Lazo; Keith Parker. Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th ed.). New York: McGraw-Hill. p. 79. ISBN 978-0-07-142280-2.
- ↑ Schlatter, J; Madras, JL; Saulnier, JL; Poujade, F (4 September 1999). "[Drug interactions with methadone].". Presse medicale (Paris, France : 1983). 28 (25): 1381–4. PMID 10506872.
- 1 2 "Carbamazepine Drug Label". http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=7a1e523a-b377-43dc-b231-7591c4c888ea. External link in
|website=(help); - ↑ Kaniwa, N; Saito, Y (June 2013). "Pharmacogenomics of severe cutaneous adverse reactions and drug-induced liver injury.". Journal of human genetics. 58 (6): 317–26. doi:10.1038/jhg.2013.37. PMID 23635947.
- 1 2 Amstutz, U; Shear, NH; Rieder, MJ; Hwang, S; Fung, V; Nakamura, H; Connolly, MB; Ito, S; Carleton, BC; CPNDS clinical recommendation, group (April 2014). "Recommendations for HLA-B*15:02 and HLA-A*31:01 genetic testing to reduce the risk of carbamazepine-induced hypersensitivity reactions.". Epilepsia. 55 (4): 496–506. doi:10.1111/epi.12564. PMID 24597466.
- ↑ Leckband, SG; Kelsoe, JR; Dunnenberger, HM; George AL, Jr; Tran, E; Berger, R; Müller, DJ; Whirl-Carrillo, M; Caudle, KE; Pirmohamed, M; Clinical Pharmacogenetics Implementation, Consortium (September 2013). "Clinical Pharmacogenetics Implementation Consortium guidelines for HLA-B genotype and carbamazepine dosing.". Clinical pharmacology and therapeutics. 94 (3): 324–8. doi:10.1038/clpt.2013.103. PMID 23695185.
- ↑ Granger P.; et al. (1995). "Modulation of the gamma-aminobutyric acid type A receptor by the antiepileptic drugs carbamazepine and phenytoin". Mol. Pharmacol. 47: 1189–1196.
- ↑ Dailey, JW; Reith, ME; Steidley, KR; Milbrandt, JC; Jobe, PC (1998). "Carbamazepine-induced release of serotonin from rat hippocampus in vitro.". Epilepsia. 39: 1054–63. doi:10.1111/j.1528-1157.1998.tb01290.x. PMID 9776325.
- ↑ Dailey, JW; Reith, ME; Yan, QS; Li, MY; Jobe, PC (11 June 1997). "Carbamazepine increases extracellular serotonin concentration: lack of antagonism by tetrodotoxin or zero Ca2+.". European Journal of Pharmacology. 328: 153–62. doi:10.1016/s0014-2999(97)83041-5. PMID 9218697.
- ↑ Kawata, Yuko; Okada, Motohiro; Murakami, Takuya; Kamata, Akihisa; Zhu, Gang; Kaneko, Sunao (2001). "Pharmacological discrimination between effects of carbamazepine on hippocampal basal evoked serotonin release". British Journal of Pharmacology. 133 (4): 557–567. doi:10.1038/sj.bjp.0704104. PMC 1572811
 .
. - 1 2 D.F. Scott. "Carbamazepine". Chapter 8 in The History of Epileptic Therapy: An Account of How Medication was Developed. History of Medicine Series. CRC Press, 1993 ISBN 9781850703914
- ↑ Schindler W, Häfliger F (1954). "Über Derivate des Iminodibenzyls". Helvetica Chimica Acta. 37 (2): 472–83. doi:10.1002/hlca.19540370211.
- ↑ Okuma T, Kishimoto A (February 1998). "A history of investigation on the mood stabilizing effect of carbamazepine in Japan". Psychiatry Clin. Neurosci. 52 (1): 3–12. doi:10.1111/j.1440-1819.1998.tb00966.x. PMID 9682927.
- 1 2 Prosser RS, Sibley PK2. Human health risk assessment of pharmaceuticals and personal care products in plant tissue due to biosolids and manure amendments, and wastewater irrigation. Environ Int. 2014 Dec 5;75C:223-233. doi: 10.1016/j.envint.2014.11.020. PMID 25486094
- ↑ drugs.com drugs.com international listings for carbamazepine Page accessed June 3, 2015
External links
| Wikimedia Commons has media related to Carbamazepine. |
- Carbamazepine overview from PsychEducation.org
- Extensive review of the effects of carbamazepine in pregnancy and breastfeeding